This leaflet contains information about clitoral reconstruction after Female Genital Mutilation (FGM). We also call this "reconstruction surgery". In this brochure we focus on the surgical procedure. Since 2010, about 50 women in the Netherlands have undergone restorative surgery. Worldwide, that is more than 10,000 women.
Amsterdam UMC is the designated center of expertise for FGM in the Netherlands. You can come to us for counseling and possible treatment/surgery.
Note: clitoral reconstruction is not the same as defibulation Defibulation involves enlarging the vaginal opening. A woman who has undergone the most severe form of FGM (infibulation) is then "reopened". This is different from clitoral reconstruction. |
For whom is the operation intended?
Reconstruction surgery is primarily for women who have been circumcised. Women who have had vulvar cancer can also undergo restorative surgery.
The clitoris
Do circumcised women have a clitoris?
Yes, circumcised women still have a clitoris. It is much larger than the "tip" visible on the outside. Most of the clitoris is on the inside of the body (see drawing). During circumcision, the visible part of the clitoris is cut off; the rest remains intact. This cannot be seen on the outside, but it is still there.
What types of Female Genital Mutilation are there?
The World Health Organization (WHO) defines 4 types of FGM:
TYPE I
Partial or total removal of (the visible part of) the clitoris or in exceptional cases only the skin fold around the clitoris (clitoridectomy).
TYPE II
Partial or total removal of (the visible part of) the clitoris and labia minora, with or without removal of the labia majora (excision).
TYPE III
Narrowing of the vaginal opening by cutting away and joining the labia minora and/or labia majora, with or without removal of the clitoris (infibulation).
TYPE IV
Any other harmful acts on the female genital organs for non-medical reasons, such as puncturing, piercing, carving, scraping and cauterizing.
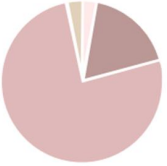 "Out of the 50 women in the Netherlands who have the
"Out of the 50 women in the Netherlands who have the
have undergone surgery, 3% had a
Type I, 18% a Type II, 76% a Type III and
 3% a Type IV circumcision."
3% a Type IV circumcision."
TYPE I
TYPE II
TYPE III
TYPE IV
"I want to feel like a woman again. There is something taken away and I want that back. I don't feel complete”.
The operation
What does the operation involve?
In clitoral reconstruction, we bring to the surface the clitoris that is still present deeper inside the body. The gynecologist first removes the scar tissue created by the circumcision. Then the clitoris is freed, brought forward and sutured into its new position. Sometimes the clitoris is covered with a piece of protective mucous membrane from the inside of the vagina. Most women choose to leave this uncovered so that the (pink) color is less noticeable later.
Can the gynecologist also make labia?
Yes, you can. Often a plastic surgeon then operates along with the gyneacologist. To make the new labia, the plastic surgeon uses a piece of skin from the buttocks. Most women choose to restore only the clitoris, not the labia.
Does the clitoris look like a "normal" clitoris after surgery?
The gynecologist tries to recreate the clitoris as closely as possible. Still, it never looks 100% the same. You will always continue to see a scar.
Is there a maximum age for the surgery?
No, there is no maximum age for recovery surgery. All women as young as 18 are eligible.
Will I have to go under anesthesia for the surgery?
Yes, general anesthesia is recommended. This will prevent you from reliving the circumcision. You can also opt for partial anesthesia (Spinal). You will always have an appointment with the anesthesiologist in which you can discuss this and ask questions.
How long will the surgery take?
Reconstruction surgery is a fairly simple procedure. It takes an average of 45 minutes to 1 hour. If the gynecologist also makes small labia, the surgery takes longer: about 1.5 to 2 hours.
Will photographs be taken?
Yes, photographs will be taken before and after reconstruction surgery. These will go into your medical record in a protected manner.
Will I get my feelings back through the surgery?
This can never be guaranteed. The experience of sexuality is determined by psychological, social and cultural factors. Scientific research shows that most women experience an improvement in clitoral pleasure.
"Some of the women are not operated on (immediately) because, for example, they have unrealistic expectations about the outcome of the surgery or there are psychological problems that need to be treated first."
Is my clitoris painful after surgery?
Yes, your clitoris may be hypersensitive immediately after surgery. The scar may also hurt.
Is there any chance of complications?
Yes, as with any surgery, there is always a chance of complications. Research shows that complications occur in 5 to 15% of surgeries. These include inflammation, bleeding, loosening of sutures and mild fever. Usually these mild complications disappear on their own after a while. Occasionally, a new surgery is required.
Why do women want reconstruction surgery?
Research shows that women mainly want to feel more feminine. In addition, they want to improve their sexual functioning and have less pain (during sex).
Are women satisfied with the surgery?
Women generally experience a positive effect. They feel more female, are more confident, have less pain and enjoy themselves more during sex. They are very happy to have had the surgery (84%). There are also women who are disappointed with the surgery.
Roadmap for clitoral reconstruction surgery
- GP: Discuss your desire for reconstruction surgery with your GP first. The family doctor will give you a referral letter. If you find this difficult, you can also contact our clinic directly and we will work with you.
- Intake: Before surgery, you usually have several conversations. The gynecologist asks what your wishes and expectations are. The gynecologist also asks questions about your psychological state, your general physical condition and sexual functioning. During the intake, you will be explained the possibilities of the surgery.
- During the intake it can be good to have a key person/interpreter present. This is so that this person can support you and translate for you (if necessary). If you prefer not to or have no need for translation, this is certainly not mandatory.
- Physical examination: You will have a physical examination. You will be given a good explanation of the findings, preferably with a mirror so you can look as wel. Do you have any further questions? If so, we will be happy to answer them.
- Consulting other specialists: Do you have psychological, physical or sexual problems? If so, you will make a separate appointment with a sexologist and/or a psychologist. During the intake we will decide together with you whether we will run this program simultaneously with any surgical procedures.
- Assessment: You will hear if you qualify for the surgery. Sometimes surgery is not (at this time) the right solution to your problems.
- Informed Consent: You will be given information before surgery about your options, limitations and risks of complications. Then you give consent for the surgery.
- Participation in research: we will ask you if you would like to participate in scientific research to make our care better. We will explain more about this at the consultation.
- Schedule date and appointment with anesthesiologist: The surgery can be scheduled. You will also have an appointment with the anesthesiologist to further discuss general anesthesia or spinal.
- Surgery: You will have surgery usually the operation is a day procedure. In principle, you can go home the same day. If you also need minor labia repair, you may stay in the hospital overnight. Plan this well and have someone pick you up.
- Surgery recovery process: You will receive a leaflet with post-surgery living rules after surgery, please read it carefully. Your wound needs to recover, in doing so you should rest as much as possible. You will be given prescription painkillers to help with the pain. Expected recovery time is often between 6-12weeks. Exactly how long it takes often varies from person to person. (See further in chapter recovery process)
- Checkups: You will come back for check up after 1 week and 3-4weeks from the day of the surgery. The gynecologist will also want to see you after 3 months- 6 months and after 1 year.
Role Key Person/Interpreter/Partners:
It is important that you feel heard, supported and safe in consultation rooms. You may always bring partners, and it is often nice to have a key person involved. A key person is a trained professional who can support you.
A key person often comes with you to your appointments such as at intake, the key person often has the same background as you and often speaks your native language. The key person performs several crucial roles:
- Educator, support person and companion: The key person can provide emotional support for you during the appointment. This may include reassuring you, encouraging communication with your doctor, and providing general guidance during the process.
- Mediator: you and your doctor often come from different backgrounds, so it is nice to have someone there who understands both cultures. They can therefore explain cultural differences (nuances/context) to both sides and thus avoid misunderstandings.
Interpreting: sometimes if you are not proficient in Dutch or English an interpreter is needed. In some cases the key person is an official interpreter in other cases we may arrange an interpreter by phone or in person. We strive for this person to be a woman, but this is not always possible.
It is very important that you have a trusting relationship with the key person (or interpreter). This helps to make the experience less stressful. It makes communication between you and the caregivers easier. If you are uncomfortable, please indicate this immediately. We can then help and support you in this.
Recovery process
How long will I have to stay in the hospital?
The surgery is usually a day surgery. You will have surgery in the morning and be allowed to go home in the evening. If you also want to have minor labia repair, some women stay in the hospital overnight.
How long should I rest?
The wound must have a week of total rest. So you should take it easy as much as possible during the first week. Making a cup of tea or taking a shower is fine. But do not, for example, go shopping, pick up the children from school, ride your bike, cook, swim or take a bath. In the following weeks, you can slowly resume your daily activities. Take it easy for at least six weeks and don't do any heavy physical work. For example, ask for help with household chores.
Will I be given medication?
For the first 6 weeks after surgery, the wound may be sensitive and painful. For example, when urinating and walking. You will be given prescriptions for painkillers and possibly an ointment. Make sure that the clitoris does not dry out. Also keep the wound clean.
How long does recovery take?
It takes 6 to 12 weeks for the surgical wound to heal completely. Exactly how long it takes cannot be said in advance. It varies from person to person.
When can I have sex again?
It is wise not to have sex until the wound is completely healed. So after 6 to 12 weeks.
What problems should I call for, what are alarm symptoms?
- You Have difficulty urinating: pee doesn't come, is very painful or you pee stinks.
- Fever (measured 38.5 degrees or more),
- The wound suddenly hurts a lot or becomes increasingly painful.
- If the wound becomes red or thick.
- If you bleed from the wound.
- If the wound smells very foul or pus is coming out.
- If you are in doubt whether what you are feeling is normal you can also consult anytime.
When should I come for a checkup?
You will come back for check up after 1 week and 3-4weeks from the day of the surgery. The gynecologist will also want to see you after 3 months- 6 months and after 1 year. If you have complaints or concerns you can always contact us earlier.
Will my family doctor also be notified?
Yes, at the end of the procedure, the gynecologist always sends a letter to your doctor with all the information. If you do NOT want this, please tell us. In this case we will not send it.
Cost
What is the cost of surgery?
The cost of the reconstruction surgery depends on the size of the procedure.
Will health insurance reimburse for the surgery?
To date, reconstruction surgery in the Netherlands is only reimbursed by health insurance company in case of medical reason (physical complaints). This means that in some cases the surgery is reimbursed by your health insurance company. Check this carefully with the gynecologist and your health insurance company.
You should keep in mind that you must pay your deductible even if you receive conservative treatment or counseling without surgery.
You also retain the cost of your transportation to appointments.
More information?
Would you like to know more about clitoral reconstruction? You can find additional information at the Amsterdam UMC website.
Or you can contact our specialized team directly at:
Phone numbers (available weekdays between 8 a.m.-5 p.m.):
General benign gynecology outpatient clinic: 020-5661601
Phone number for questions about FGM care 020-5667525
(If no answer, please leave a voicemail with your name and phone number and you will be called back)
Email: VGV@amsterdamumc.nl
